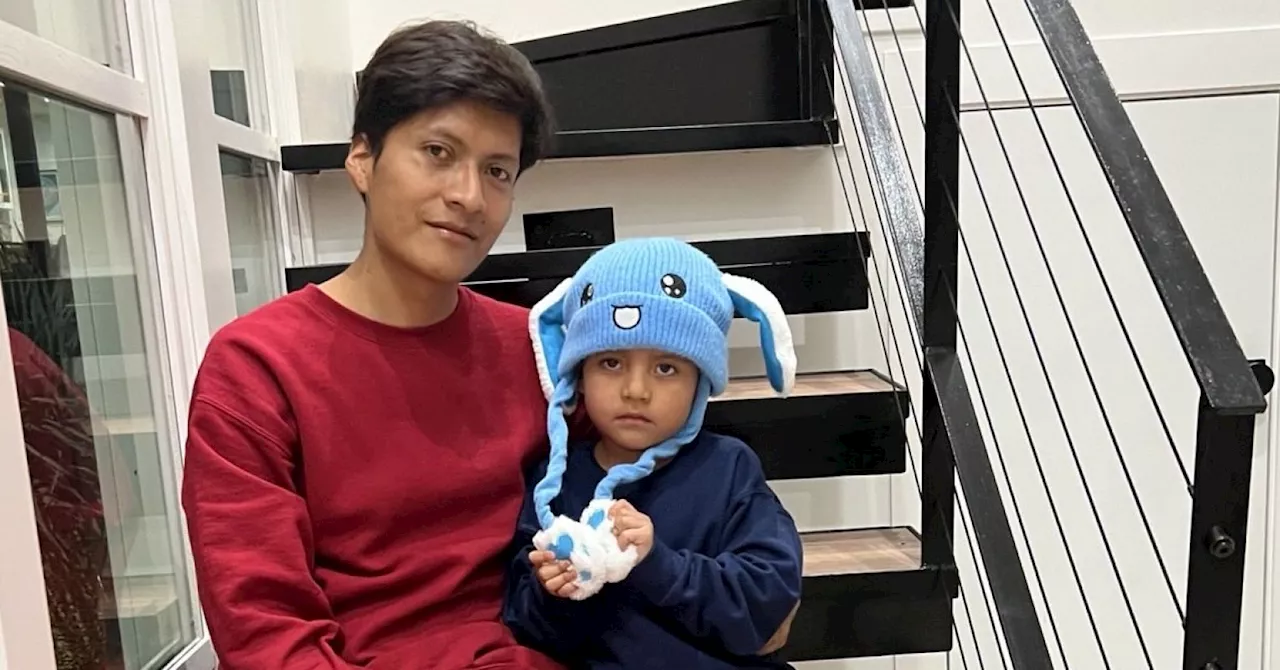
The separation of families, particularly children from their parents, is increasingly being scrutinized by mental health professionals. This scrutiny comes in the wake of incidents like the detention of five-year-old Liam Conejo Ramos, who was taken into custody by Immigration and Customs Enforcement (ICE) in January 2026. Liam, alongside his father, was detained shortly after arriving at their Minneapolis home, igniting national outrage over the treatment of families seeking asylum.
Family separation, even when framed as a safety measure, can have severe consequences on a child’s mental health. Research indicates that children who experience such separations often develop post-traumatic stress disorder (PTSD), anxiety, and depression. The psychological toll extends beyond individual cases, impacting entire communities, particularly those consisting of Black and Brown families, who are disproportionately affected by these practices under the guise of child welfare and juvenile justice.
Concerns about immigration status can also lead to decreased healthcare utilization and diminished school attendance, further complicating a child’s development and well-being. One tragic account involves a child whose family faced threats of deportation, ultimately leading to her tragic death. Such incidents highlight the urgent need for mental health providers to reconsider their roles in legitimizing practices that facilitate family separation.
In many cases, mental health providers unknowingly contribute to a system that perpetuates trauma. Through mandated reporting and diagnoses that can criminalize typical childhood behavior, such as oppositional defiant disorder, providers often funnel families into systems that undermine their stability. This is particularly concerning as children in psychiatric facilities or juvenile detention centers may face coercive practices that exacerbate their mental health issues.
The historical context of these practices reveals a troubling legacy. The mental health profession, which emerged in the mid-20th century, often focused on the perceived deficiencies of children from marginalized backgrounds. This approach has evolved, but the fundamental logic remains: systems of care frequently operate under the assumption that separation is necessary for safety, despite overwhelming evidence of the harm it causes.
A study highlighted the circular logic within child welfare research, demonstrating how interventions are often developed within the very institutions that perpetuate harm. For instance, one study indicated that Black parents receiving training while under surveillance experienced depression, yet the solution proposed was to add depression treatment rather than address the root causes of their distress, including the surveillance itself.
While mental health providers may believe they are helping children in need, their involvement can inadvertently support the notion that healing is possible in detention settings. This contradicts established principles regarding trauma and safety. The challenge lies in redefining care; instead of viewing detention as a place of healing, mental health professionals must advocate for preventive measures that keep families together.
Redirecting funding from child detention facilities to community support systems could fundamentally alter the landscape of care. Initiatives like California’s Differential Response and New York’s Family Assessment Response provide voluntary supports rather than punitive investigations, showcasing alternatives to the current system.
The urgent need for change is underscored by the emotional distress witnessed in detention facilities. In the days leading up to Liam’s release, reports surfaced of children pleading to be freed from their confinement. This serves as a poignant reminder of the psychological harm inflicted by family separation, which resonates across various systems, including immigration and juvenile justice.
Mental health professionals are thus called upon to recognize their complicity in these systems and to champion initiatives that prioritize family unity. By redirecting research and resources towards community-based supports, providers can play a crucial role in dismantling the current framework that permits separation.
As the movement towards mental health rights and recovery gains momentum, community-based alternatives are emerging. Peer respite centers and diversion programs that keep youth within their communities are examples of how care can be reimagined. The ongoing closures of juvenile detention facilities highlight that detention is a policy choice, not an inevitable necessity.
The mental health community has an ethical obligation to confront these practices. Healing cannot occur within the confines of a detention facility. It is imperative that mental health providers shift their focus towards preventing family separation and advocating for policies that support the well-being of children and their families. The time for change is now, and the commitment to keeping families together must be prioritized as a fundamental aspect of mental health care.