A recent study by researchers from Yale University and the Karolinska Institutet in Sweden has revealed significant similarities between the molecular changes that occur in brain inflammation and those that happen during normal brain development. The findings, published on March 15, 2024, hold promise for advancing treatment options for multiple sclerosis, a disease in which the immune system erroneously attacks nerve cells in the brain.
The study’s lead researcher, Gonçalo Castelo-Branco, who is affiliated with the Karolinska Institutet, emphasized the importance of this basic research in understanding how certain cells contribute to disease progression. In a recent interview, he stated, “With this kind of research, we understand better the property of the cells that are the major players in disease evolution.”
A key aspect of the study involved the development of a new analytical technique termed “spatial tri-omic,” which builds on existing technologies that utilize unique DNA barcodes to map molecules in tissues. Traditional methods typically measure only one property of a cell, but spatial tri-omic allows researchers to assess multiple characteristics simultaneously, including gene activity, RNA expression, and protein production.
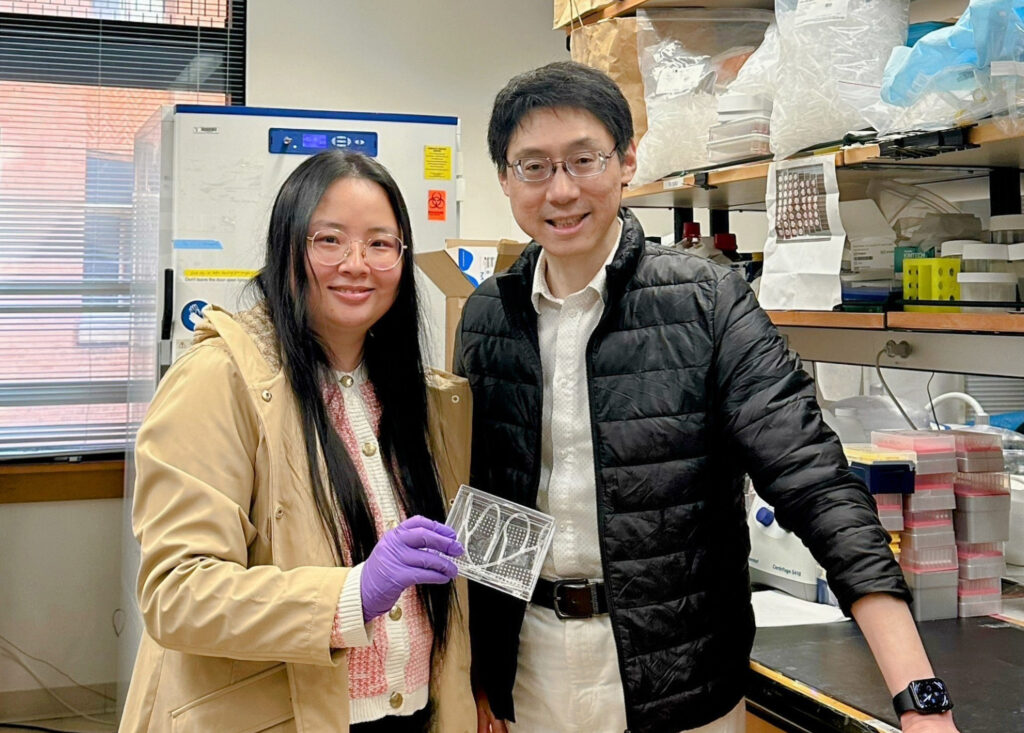
The researchers conducted detailed examinations of mouse brains and human brain tissue, discovering shared patterns in development and inflammation. Co-head of the study, Di Zhang, explained that microglial cells—crucial for brain development—also play a role in neuroinflammatory processes. This observation suggests that the brain employs similar genetic and molecular mechanisms for both development and self-repair following inflammation.
Zhang articulated the significance of the study, stating, “In this study, we used spatial multi-omics to capture the brain’s journey of creation and self-healing — development, myelination, inflammation, and repair, not as separate chapters, but as movements of the same symphony of time.”
The implications of these findings extend to the treatment of multiple sclerosis. When neuroinflammation disrupts myelination, the protective sheath surrounding nerve fibers is compromised. This process is vital for brain development and functions such as learning and motor control. In multiple sclerosis, the immune system’s attack on the myelin sheath exacerbates chronic neuroinflammation, leading to further damage.
Castelo-Branco noted that prior medications for multiple sclerosis primarily targeted the immune system, proving effective only in the early stages of the disease. He suggested that insights from this research could inform the development of new therapies that focus on the affected tissue itself, stating, “This is why these kinds of studies are important because then we can start understanding better how these molecules might be acting in the target tissue.”
Zhang also highlighted the potential for improved therapeutic strategies and drug development for not only multiple sclerosis but also other neuroinflammatory and neurodegenerative diseases. Her future research plans include further investigation of human brain tissue and exploring applications related to conditions such as Alzheimer’s and Parkinson’s disease. Furthermore, she mentioned that the spatial technology could be adapted for studying small tissue samples from various organs, including the heart, lungs, and intestines.
The Yale Department of Biomedical Engineering, which has been at the forefront of such innovative research since its establishment in 2003, continues to contribute to the understanding of complex biological processes and their implications for human health.
This groundbreaking study not only enhances the understanding of brain development and inflammation but also paves the way for potential advancements in treating debilitating conditions like multiple sclerosis and beyond.