A recent study from the University of Rochester Medical Center has unveiled a potential breakthrough in the identification and treatment of bone infections caused by the bacterium Staphylococcus aureus. Researchers have identified a small protein, known as CCL20, that may serve as both a diagnostic tool and a target for treatment, offering hope for patients suffering from osteomyelitis and other related infections.
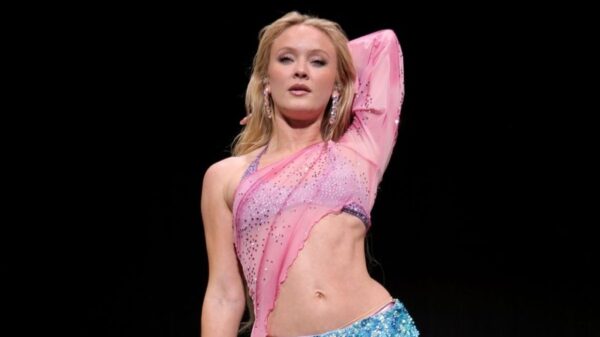
The study, published in the journal mBio, highlights the role of CCL20 in the body’s immune response to bacterial infections. The research team observed that levels of CCL20 increased significantly in mice infected with Staphylococcus aureus. Mice lacking this chemokine exhibited more severe infections and larger abscesses, suggesting its crucial role in the immune response to infection.
Potential Diagnostic Tool for Early Detection
The findings indicate that CCL20 could serve as a biomarker for detecting bone infections early. Healthy patients who had undergone hip or knee replacements showed normal levels of CCL20, but those who developed infections experienced a fivefold increase. Alarmingly, patients who succumbed to sepsis had CCL20 levels that were 100 times higher than normal, pointing to its potential as an SOS signal to the immune system.
Dr. Gowrishankar Muthukrishnan, an assistant professor in Orthopedics and Microbiology & Immunology at the University of Rochester’s Center for Musculoskeletal Research, emphasized the urgency of rapid diagnosis and treatment for staph infections. “Treating a staph infection quickly offers patients the best chance at recovery and can prevent the risk of sepsis, which can cause death in a matter of hours,” he stated. Current diagnostic methods for bone infections are inadequate, and improvements in surgical outcomes have stagnated for over two decades.
The Economic Impact of Bone Infections
Bone infections represent a significant healthcare burden, especially for the approximately 2 million total joint replacements performed annually in the United States. While these surgeries are generally successful, complications such as osteomyelitis can lead to severe outcomes, including the need for additional surgery or prolonged antibiotic treatment. The risk of reinfection stands at nearly 50% once an infection occurs.
With an aging population and a projected increase in joint replacements, the incidence of prosthetic joint infections could reach 200,000 annually by 2030. The total healthcare costs associated with bone infections are estimated to soar to $3 billion per year during that period, indicating a pressing need for effective diagnostic and treatment strategies.
Dr. Himanshu Meghwani, the study’s first author and a staff scientist at the Center for Musculoskeletal Research, suggested that CCL20 might also be leveraged as a therapeutic agent. By enhancing the recruitment of immune cells to infection sites, it could potentially bolster the body’s natural defenses against bacterial infections. However, the researchers acknowledged that further investigation is required, as some patients with high CCL20 levels still struggle to combat infections effectively.
In conclusion, the identification of CCL20 as both a biomarker and a potential treatment avenue could revolutionize the management of bone infections, ultimately improving outcomes for countless patients. Continued research in this area is essential to fully understand the implications of CCL20 and to develop targeted therapies that can mitigate the risks associated with these debilitating infections.