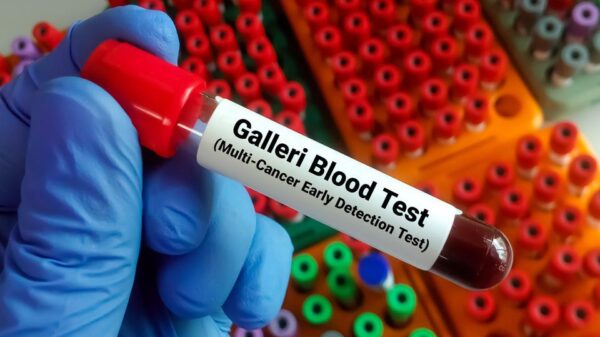
The Galleri cancer test, a blood test designed to detect hidden cancers at an early stage, is set to gain significant attention during this year’s Super Bowl with a nationwide commercial. Priced at $949 and marketed by companies such as Hims & Hers, the test analyzes cell-free DNA in the blood to identify specific methylation patterns associated with cancer. Individuals can purchase the test online, visit a designated testing center for a blood draw, and receive results within approximately two weeks. The outcomes indicate either “cancer signal detected” or “no cancer signal detected.” In real-world usage, about 1 in 100 individuals receive a positive signal.
Galleri claims to help determine the likely tissue of origin for positive results, such as pancreatic or colon cancer, guiding further investigations. The manufacturer, GRAIL, recommends the test for adults aged 50 and older, or those with elevated cancer risk factors, including smoking, personal or family history of cancer, obesity, or genetic predisposition. However, it is crucial to note that the test’s effectiveness has not been thoroughly studied across these varying demographics.
Despite its promising concept, experts urge caution. The fundamental questions surrounding the test are whether it truly works and if it contributes to a longer, healthier life. Current evidence suggests that while multi-cancer early detection tests like Galleri are innovative, their potential drawbacks for most individuals may outweigh the benefits.
Concerns Over Reliability and False Positives
The efficacy of any cancer test hinges on its ability to accurately predict the presence or absence of cancer. Unfortunately, Galleri’s performance reveals significant limitations. The test is less effective at detecting early-stage cancers when timely intervention is critical. In a validation study, the sensitivity for Stage I cancers was only 16.8%, contrasting sharply with over 90% for Stage IV cancers.
Moreover, Galleri presents a considerable false positive challenge. With a specificity rate of about 99%, the test appears reliable at first glance. However, in a study known as the PATHFINDER trial, 62% of positive results were false alarms, leading to unnecessary follow-up tests such as CT, MRI, and PET scans, as well as invasive procedures like endoscopies or biopsies. This diagnostic odyssey can span an average of six months, resulting in emotional distress and financial burdens for patients—many of whom ultimately do not have cancer.
Even in cases where the test returns negative results, caution is warranted. The PATHFINDER study revealed that 71% of cancers diagnosed during the research were identified through traditional screening methods or symptomatic presentations rather than through Galleri. A negative result may create a misleading sense of security, potentially leading individuals to neglect standard screenings or dismiss emerging symptoms. It is vital to understand that a negative Galleri test does not replace guideline-recommended screenings like colonoscopies, mammograms, or lung cancer CT scans.
Evaluating the Broader Implications of Galleri
While there are cases where Galleri has proven beneficial, such as in the detection of early, treatable gastric cancers in specific patients, broader applications remain uncertain. Many cancers identified by Galleri, including gastric, pancreatic, or ovarian cancers, currently lack population-level screening guidelines. This aspect represents a unique opportunity, yet its ability to facilitate early diagnoses in a way that improves overall outcomes remains unknown.
A significant concern is the absence of randomized controlled trials demonstrating that Galleri testing reduces cancer mortality. The medical community has encountered numerous screening tests that, while effective in detection, have not contributed to improved survival rates. For this reason, large-scale studies like the UK’s NHS-Galleri study, involving 150,000 participants, are crucial for addressing these concerns.
Another challenge is what has been termed the “diagnostic black hole.” Clinicians may face dilemmas when Galleri indicates a potential cancer signal, yet subsequent imaging tests yield no findings. Currently, there is no standard protocol for determining how long or how aggressively to pursue further diagnostics, leaving patients in limbo and increasing levels of anxiety.
Additionally, the cost of Galleri may exacerbate existing disparities in healthcare access. At $949, the test primarily caters to those with disposable income, potentially sidelining vulnerable populations who cannot afford it, even as proven screening methods remain underutilized in these communities.
Given these complexities, major professional medical societies have refrained from recommending multi-cancer early detection tests for routine screening. Organizations emphasize that rigorous validation through ongoing trials is essential, and these tests should not be considered a standard of care.
Despite the limitations, some patients may still opt for the Galleri test, driven by a desire for comprehensive health information. Some healthcare providers, particularly in concierge or direct-pay models, might advocate for its use. For those who choose to undergo the test, a thorough pre-test consultation with a qualified healthcare professional is essential. This discussion should clearly outline the statistics, including risks associated with false negatives and false positives, and establish a plan for the subsequent diagnostic process following a positive result.
The ambition to catch multiple cancers early through a simple blood test is an exciting frontier in medical science. However, current methodologies and validations fall short of the promise. Until future iterations of blood-based tests for multi-cancer early detection demonstrate improved accuracy and patient outcomes, individuals should prioritize proven cancer prevention strategies. Staying up-to-date with guideline-recommended screenings, refraining from smoking, maintaining a healthy weight, moderating alcohol consumption, and addressing persistent symptoms are the most effective measures for reducing cancer risk.