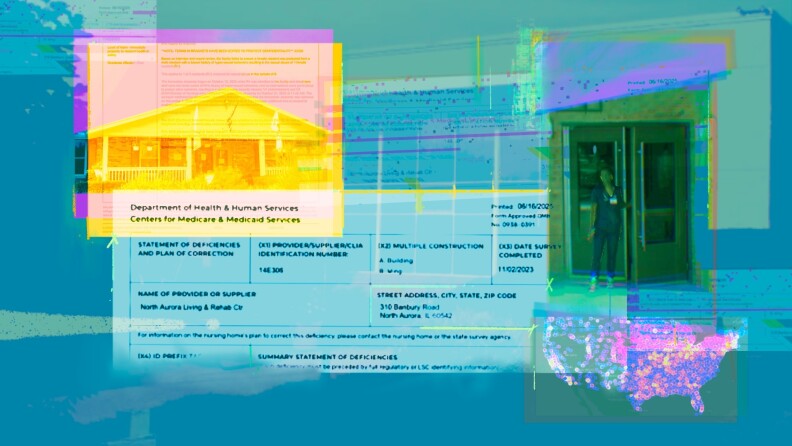
Concerns about the treatment of individuals with mental illnesses in nursing homes have intensified following a distressing incident at the North Aurora Care Center in Illinois. In October 2023, the facility admitted a 28-year-old man, referred to as V.R., diagnosed with schizophrenia and cognitive delays. Despite staff reservations about his admission, corporate officials from Petersen Health Care overruled these concerns. Less than 24 hours after his arrival, V.R. allegedly groped a resident and attempted to engage in inappropriate behavior with others.
This incident highlights a troubling trend in nursing homes nationwide, where the care and safety of residents, particularly those with serious mental illnesses, are increasingly jeopardized. According to an investigation by the APM Research Lab, a significant number of nursing home residents—approximately 1 in 5—are living with serious mental illnesses, such as schizophrenia or bipolar disorder.
Widespread Issues in Care Facilities
The challenges associated with caring for individuals with mental health issues are well-documented. Many nursing homes are not equipped with the specialized staff or training needed to address the unique needs of these residents. In Illinois, a 2010 law mandated the establishment of a certification program for nursing homes that would allow them to admit residents with serious mental illnesses. However, nearly 15 years later, the state has not certified any facility under this requirement, despite a significant proportion of nursing home residents in Illinois being there primarily due to mental health issues.
By late 2023, around 70% of residents at North Aurora were reported to have mental health conditions, yet there is no record of the facility being certified. The Illinois Department of Public Health has not provided an explanation for this oversight.
Research indicates that nursing homes are often ill-suited for the complex needs of individuals with mental illnesses. Many residents receive inadequate care, which can exacerbate their conditions, leading to a cycle of institutionalization that is difficult to escape. A lack of community-based services, long waitlists, and financial instability can push vulnerable individuals into nursing homes, where they often do not receive the appropriate treatment.
Consequences of Inadequate Oversight
Abuse and neglect in nursing homes are prevalent, particularly in facilities that serve a high proportion of residents with mental illnesses. APM Research Lab’s findings suggest a correlation between the percentage of residents with mental health issues and the frequency of abuse citations. Furthermore, poorly staffed facilities are more likely to experience incidents of abuse, whether perpetrated by residents or against them.
For instance, a resident with serious mental illness in Kansas City, Missouri, reportedly attacked a physically frail resident, leading to the latter’s death. In another case, a resident in Louisiana died after being left unsupervised while smoking outside at night. These incidents underscore the risks faced by vulnerable individuals in under-resourced environments.
Despite these alarming statistics, financial penalties for nursing homes that fail to provide adequate care are often minimal or non-existent. For example, North Aurora Care Center has faced fines for failing to meet staffing requirements and for neglecting the nutritional needs of residents, yet has not been penalized for the serious incident involving V.R. This lack of accountability raises concerns about the effectiveness of regulatory oversight.
The nursing home industry is also financially burdened, with taxpayers often footing the bill. The average cost for a nursing home resident is approximately $6,000 per month, with federal programs like Medicare and Medicaid covering a significant portion of these expenses. Most facilities housing a high number of residents with serious mental illnesses are owned by for-profit companies, which tend to report a higher incidence of abuse compared to non-profits or government-operated facilities.
In response to these systemic issues, advocates for mental health care are pushing for improved services and funding for community-based treatment options. U.S. Representative Daniel Goldman has proposed legislation to facilitate Medicaid funding for at-home mental health care, emphasizing the need for a shift away from institutionalized care.
The distressing case of V.R. serves as a reminder of the ongoing struggles faced by individuals with mental illnesses in nursing homes. As the system continues to grapple with these complex challenges, the need for comprehensive reforms becomes increasingly urgent.
V.R. has since been committed to a state-run treatment center, where he will receive care tailored to his needs. His case exemplifies the critical gaps in the current system and the urgent need for better support structures for individuals with serious mental health conditions.