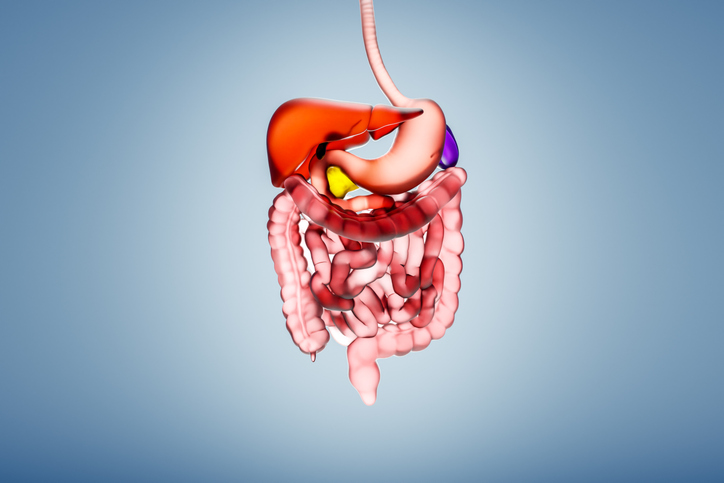
The management of gastrointestinal (GI) conditions is undergoing significant evolution, driven by advancements in understanding the gut microbiome and increased public interest in gut health. Over the past ten years, conditions such as irritable bowel syndrome (IBS) have shifted from being perceived as psychological issues to recognized physical health concerns. This transformation is attributed to both consumer demand for improved gut health and enhanced medical knowledge, facilitated by technological advancements.
Integrating Nutrition into Gastroenterology
A growing recognition of nutrition’s critical role in health has led to the integration of dietary approaches in gastroenterology. Innovative diets, such as Low FODMAP and Low Fermentation Eating, are designed to manage symptoms of IBS and Small Intestinal Bacterial Overgrowth (SIBO). This shift towards a food-as-medicine initiative emphasizes the importance of nutrition in health care, advocating for the inclusion of dietary strategies in patient care plans.
The rise of gastrointestinal registered dietitians (GRDs) reflects this integrated approach. These specialists work alongside gastroenterologists to develop tailored diet plans that address individual GI health needs. By combining pharmaceutical treatments with nutritional counseling, patients can achieve more effective long-term management of their conditions. This collaboration not only helps reduce flare-ups but also minimizes future medical costs.
A notable example of this approach can be seen in the treatment of SIBO. Traditionally, antibiotics were the primary treatment, achieving a mere 44% eradication rate. In contrast, a palatable elemental diet formulation has demonstrated an impressive 83% success rate in eradicating SIBO, showcasing the potential of nutrition-based solutions in enhancing patient outcomes.
Technological Advancements in GI Diagnostics
Technology plays a pivotal role in improving care for patients with GI disorders. Recent developments in gut diagnostic technology have made it possible to deliver quicker and more accurate diagnoses at reduced costs. A landmark innovation was the introduction of the first three-gas breath test in 2020, which allows for non-invasive evaluation of hydrogen, methane, and hydrogen sulfide exhalation. This method simplifies the identification of conditions like SIBO and intestinal methanogenic overgrowth (IMO), which were previously diagnosed based on symptoms alone.
With these advancements, patients can now access at-home testing options, circumventing the lengthy wait times often associated with invasive procedures. This accessibility not only reduces the financial burden on patients but also alleviates the discomfort of waiting for essential diagnoses.
Furthermore, the emergence of mobile applications has enhanced integrated care plans for GI patients. Some of these apps, approved by the FDA, provide virtual support for managing lifestyle factors that can exacerbate chronic conditions. For instance, gastroenterologists can recommend these applications to help patients with meal planning and mindfulness techniques aimed at reducing stress, which is known to worsen symptoms of IBS.
Navigating Consumer Trends and Education
Consumer trends highlight the growing interest in health products touted by social media influencers, often leading to confusion around effective treatments for GI disorders. Products like prebiotics and probiotics have surged in popularity, with many patients believing they are panaceas for gut health. While occasional use of probiotics can be beneficial, a lack of understanding about individual microbiome needs can lead patients to choose inappropriate supplements that may exacerbate their conditions.
Gastroenterologists often find themselves addressing the consequences of these trends, helping patients discern fact from fiction. As new health fads emerge, such as the recent curiosity around consuming dirt, medical professionals must stay informed to provide accurate guidance. Increased advocacy from health experts on social media aims to counteract misinformation and promote evidence-based solutions.
As the field continues to evolve, there is potential for further growth in the management of GI disorders. Advances in diagnostic methods, integrated care strategies, and nutrition-focused approaches are transforming patient experiences. While academic research delves deeper into the complexities of the gut microbiome, health policies and insurance providers need to adapt to support these innovations effectively.
In conclusion, the landscape of gastrointestinal care is changing for the better. By embracing a collaborative approach that includes nutrition education and advanced technology, healthcare providers are improving the quality of life for patients suffering from chronic GI conditions. Continued efforts to educate patients and align treatments with clinical evidence are essential as the intersection of consumer trends and medical care continues to evolve.