A troubling gap exists in Arizona’s Medicaid coverage that forces many patients to wait until their health deteriorates before gaining access to essential weight-loss medications. For individuals like 32-year-old Jesse Lopez from Glendale, the situation is dire. After battling weight gain linked to schizophrenia treatment, Jesse’s struggle with obesity led to a diagnosis of Type 2 diabetes, which subsequently allowed him to qualify for coverage of medications such as Trulicity.
Despite the initial success of the treatment, which helped Jesse lose 15 pounds and stabilize his blood sugar levels, his eligibility for the medication disappeared once his diabetes came under control. “It’s like a tug of war,” said his mother and caregiver, Karina Lopez. “I’m going to wait for you to get sick again to give it back to you.” This reflects a broader issue where Arizona, along with 31 other states, limits Medicaid coverage of glucagon-like peptide-1 agonists (GLP-1s) strictly to patients with specific conditions like diabetes, heart failure, or hypertension.
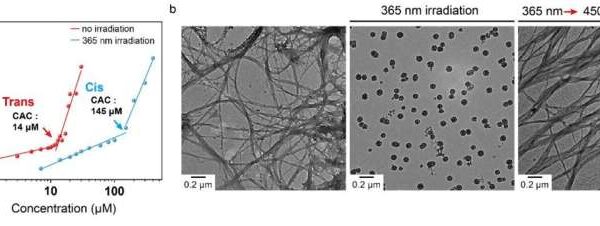
For many low-income Arizonans, the high cost of these medications—over $1,000 a month—remains a significant barrier. In stark contrast, similar treatments are markedly cheaper in other countries, with Ozempic priced at about $969 in the U.S. compared to $155 in Canada and $59 in Germany. These prices raise concerns about the accessibility of life-saving medications for those who need them most.
Legislative Efforts and Challenges
In January, state representative Amish Shah proposed legislation aimed at mandating Medicaid coverage for FDA-approved weight-loss drugs, including GLP-1s. According to the Joint Legislative Budget Committee, approximately 282,000 to 730,000 of Arizona’s 2.1 million Medicaid recipients could benefit from this coverage. The estimated cost to state taxpayers could range from $192 million to $496 million annually, with the federal government potentially contributing up to $2 billion. Unfortunately, Shah’s bill failed to advance in committee.
Many patients are left feeling trapped as they witness their health decline while waiting for necessary treatment options. Angela Rich, a 44-year-old from Mesa who has struggled with weight due to lipedema, voiced her frustration after her doctor prescribed Wegovy—only for her to learn that her Medicaid plan would not cover it. “I’m stuck. That’s what it feels like,” she said, highlighting the emotional toll of navigating a system that often seems designed to respond only after a health crisis has occurred.
Broader Implications and Patient Advocacy
The prohibition of GLP-1 coverage for weight loss under Medicare since 2003 underscores the systemic issues affecting not only low-income patients but also those on Medicare. This restriction has implications for individuals like Melissa Cox, a 52-year-old Medicare enrollee with schizophrenia, whose family faces similar struggles to secure necessary medications without a diabetes or cardiovascular diagnosis.
Lawmakers have also expressed frustration regarding the high costs of these medications. During a Senate hearing on September 24, Bernie Sanders, chair of the Health, Education, Labor and Pensions committee, confronted Lars Fruergaard Jørgensen, CEO of Novo Nordisk, which manufactures Ozempic and Wegovy. Sanders called for urgent action to address the exorbitant prices, stating that the current system risks “bankrupting” Medicare.
As Jesse continues to face challenges in maintaining his health without reliable access to medication, his mother is left to wonder how many more cycles of weight gain and loss her son will endure. “It’s literally life or death,” Karina Lopez said, reflecting the urgent need for reform in medication access policies that prioritize health outcomes over bureaucratic constraints.
The struggle for comprehensive coverage of weight-loss medications in Arizona highlights not only the urgent need for policy reform but also the deeply personal impact of these healthcare decisions on individuals and families.