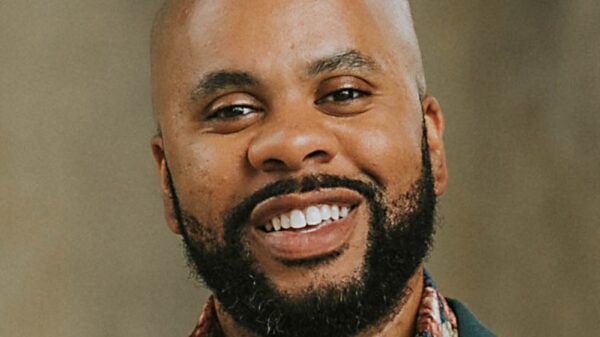
The year 2025 has emerged as a pivotal time for incretin-based therapies, particularly GLP-1 receptor agonists, in the treatment of diabetes and related conditions. Significant regulatory approvals and clinical trials have reshaped treatment protocols, highlighting the versatility of these medications across various specialties. This transformation was thoroughly examined in a recent episode of Diabetes Dialogue, hosted by Diana Isaacs, PharmD, and Natalie Bellini, DNP, who discussed the impact of these advancements on patient care.
One of the most significant developments in early 2025 was the FDA’s approval of semaglutide for patients with type 2 diabetes and chronic kidney disease (CKD), based on the findings from the FLOW trial. This trial established renal protection as a primary benefit of semaglutide, marking a critical shift in treatment algorithms. Isaacs noted that the evidence demonstrated GLP-1 receptor agonists can effectively slow the progression to advanced CKD, even in cases where SGLT2 inhibitors are not tolerated. This advancement fosters greater confidence in combination therapies.
The episode also addressed the relief brought about by the end of a global semaglutide shortage in February 2025. Prior to this, clinicians had to frequently switch patients between medications due to limited availability. Bellini recounted instances where patients were moved between different dosages, causing disruptions in treatment continuity. The decision by Novo Nordisk to increase production significantly alleviated these pressures, leading to a reduction in reliance on compounding pharmacies.
In March, the conversation shifted to the STRIDE trial, which demonstrated that semaglutide significantly improved pain-free walking distance in patients suffering from peripheral artery disease. This finding underscores the role of GLP-1 agents as essential cardiometabolic therapies, particularly given the accessibility of walking as a functional endpoint. Additionally, the trial brought attention to the cardiovascular risks associated with diabetes, reinforcing the need for integrating GLP-1 agents into cardiovascular care.
The annual ADA Scientific Sessions in June showcased a wave of incretin-related data. The discussion highlighted several promising candidates, including the monthly GLP-1 formulation, MariTide, which showed a potential weight loss of approximately 16% in early studies. Another notable mention was orforglipron, an oral GLP-1 therapy that delivered substantial reductions in A1c levels and weight without strict dosing-timing constraints. The dual amylin/GLP-1 combination, Cagri-Sema, also featured prominently, achieving over 20% weight loss in non-diabetic individuals and nearly 14% in those with type 2 diabetes.
As the year progressed, July brought top-line results from the SURPASS-CVOT. While tirzepatide did not outperform dulaglutide, it achieved cardiovascular noninferiority, enhancing clinical confidence in its use for patients at elevated cardiovascular risk. The data suggested a potential 28% reduction in three-point major adverse cardiovascular events and a 39% decrease in all-cause mortality compared to a placebo. Further analyses indicated a slowdown in estimated glomerular filtration rate (eGFR) decline among high-risk CKD populations, broadening the therapeutic rationale for using this medication.
August marked another milestone with the FDA approval of semaglutide for metabolic dysfunction-associated steatohepatitis (MASH), becoming the second therapy approved for this condition. This approval has prompted changes in clinical workflows, including more comprehensive screening and routine incorporation of FIB-4 scoring, which supports the use of GLP-1–based therapy for metabolic liver disease. Concurrently, orforglipron demonstrated a 12% weight loss in obesity trials, suggesting its potential for widespread application.
By October, oral semaglutide gained its own cardiovascular-risk-reduction indication through the SOUL trial, addressing long-standing concerns regarding the cardiovascular efficacy of oral formulations. This development opened new treatment pathways for patients who prefer or cannot use injectable therapies. Currently, semaglutide remains the only oral GLP-1 receptor agonist available, but the promising results from the SOUL trial indicate a bright future for oral therapies.
The year concluded with news from November regarding the disappointing termination of Novo Nordisk’s oral semaglutide trial for Alzheimer’s disease. The trial failed to show a statistically significant effect on slowing disease progression. Nonetheless, experts suggested that earlier intervention or the use of injectable formulations may be pivotal for future studies targeting neurodegenerative pathways.
In a final discussion, Isaacs and Bellini reflected on new findings from the SURMOUNT-4 trial, revealing that over 80% of individuals who withdrew from tirzepatide regained at least 25% of their prior weight loss, along with a reversal of cardiometabolic improvements. They reiterated the crucial message that obesity is a chronic disease necessitating ongoing treatment. The cumulative benefits of incretin-based therapies across renal protection, cardiovascular risk reduction, liver disease management, and weight control reinforce the importance of sustained, long-term treatment strategies.